By Keisha McLean, COMMUNITY ADVOCATE: Disability, Resource, Referral, Vulnerable Adult Outreach & Support
The Black Panther Party, during the Civil Rights Movement, coined the term “Survival Programs Pending the Revolution.” They recognized that what others may consider social service, are
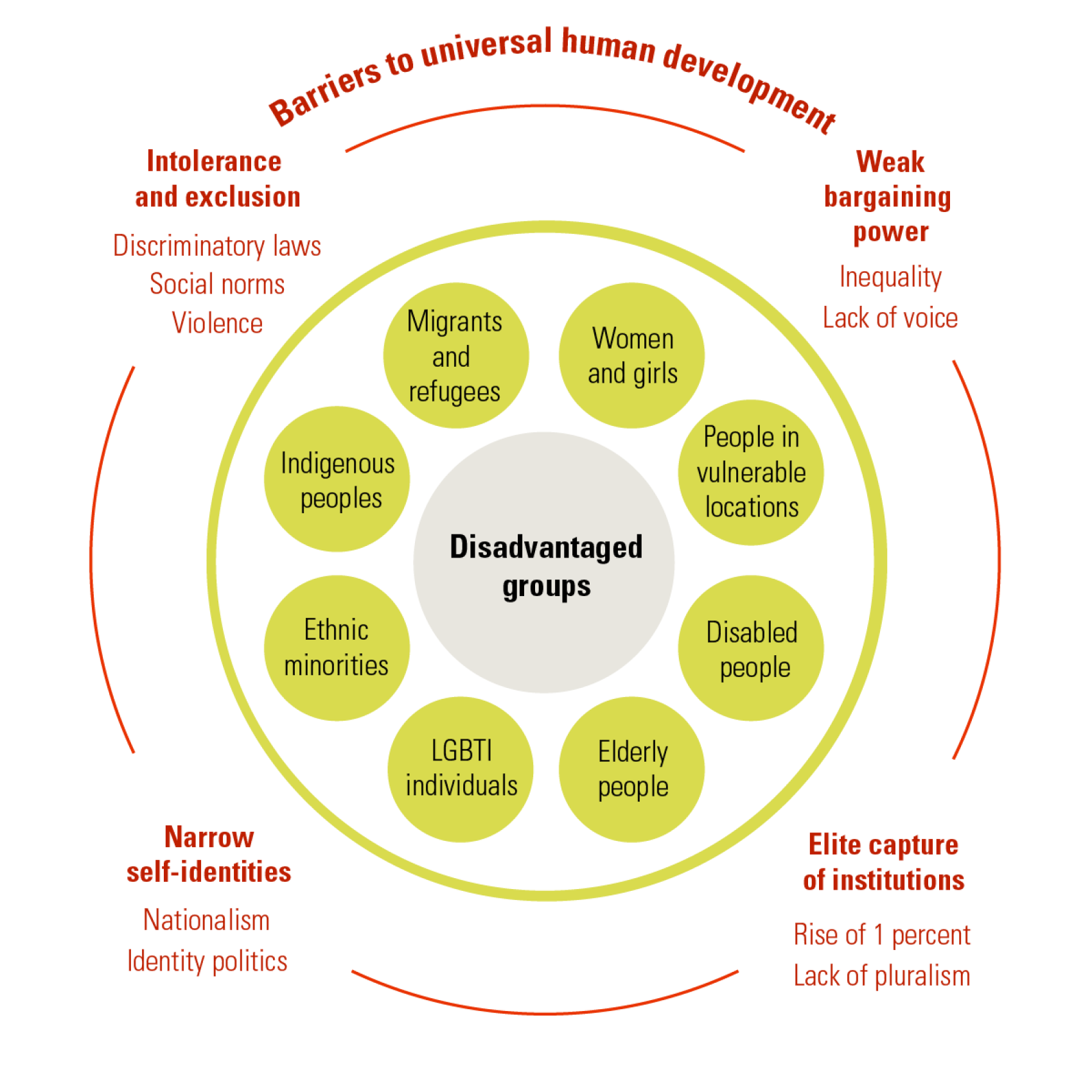
efforts that would not be needed should government and community systems work to meet the needs of their population. 41 years after the Party dissolved, in a small city in Canada, we are confronted with the same barriers for our community members: food insecurity, housing insecurity, inequitable access to health care, racism and classism, and of course, poverty. As Community Advocates, we recognize that one of our primary objectives is to support people in navigating complex systems, which means we must become incredibly knowledgeable in said systems.
An overwhelming phrase we hear is “These forms and systems are just so confusing, I’m so happy to have someone help me with the process.” To be perfectly clear, these systems we are
supporting people with are publicly accessed programs like Canadian Pension Plan, Persons with Disability, EI, Health Care, Mental Health care, Substance Use supports… etc. Programs
and systems that are supposed to support folks experiencing barriers and vulnerabilities become so complex that we then need to create a new program just in order to access these systems. It begs a simple question… why?
Through my work supporting individuals in the vulnerable adult sector, I see a reoccurring theme… the systems just aren’t set up to support the people they are supposedly built for. This
leaves the burden of systemic flaws on the shoulders of roots-based organizations, underfunded nonprofits, and overworked front line employees. The common theme is this: it’s not
sustainable.
In 2016, 20.6% of Black Canadians reported living in housing below standards, which means their housing costs more than they can afford, and/or is crowded, and/or requires major repairs. 7.7% of White Canadians reported living in housing below standards. Among Black Canadians: 12.9% were living in crowded conditions (compared to 1.1% of White
Canadians)
8.4% were living in homes in need of major repairs (compared to 6.2% of White Canadians)
28.6% were living in unaffordable housing (compared to 16.1% among White Canadians)
Between 2009 and 2012, Black Canadians reported moderate or severe household food insecurity 2.8 times more often than White Canadians. Black Canadian youth aged 12-17
reported moderate or severe household food insecurity 3.0 times more often than White Canadian youth
SOURCE:
https://www.canada.ca/en/public-health/services/health-promotion/population-health/what-determines-health/social-determinants-inequities-black-canadians-snapshot.html
In 2021, over one in six Indigenous people (17.1%) lived in crowded housing that was considered not suitable for the number of people who lived there.
In 2021, 16.4% of Indigenous people lived in a dwelling that was in need of major repairs.
SOURCE:
https://www12.statcan.gc.ca/census-recensement/2021/as-sa/98-200-X/2021007/98-200-X2021007-eng.cfm
These quick stats provide some context – how do we help people navigate systems that are inherently built to continue the status quo of marginalization? I provide outreach services to
folks experiencing housing insecurity, as well as in supportive housing facilities. Through this work, I support a lot of individuals who engage in substance use. Weekly, I hear a number of
folks expressing severe physical health concerns: open wounds, extreme mobility limitations, broken or sprained limbs, the list goes on. The next logical step is to encourage an ER visit or,
at the very least, an appointment with their GP. While the majority of people in my community don’t have access to primary care, we are left with ER or Urgent Care. And when these
concepts are presented, the people I support immediately coil at the idea of entering a clinical environment that they feel will immediately discriminate against them because of their
substance use.
“In many settings, PWID (People who inject drugs) face barriers to accessing health and social services at multiple levels, with some difficulties attributed to their distinct health conditions.
These include: early HCV treatment guidelines which exclude PWID (Kensington, 1997); clinicians who withhold antiretroviral therapy (ART) from HIV-infected PWID (Westergaard et al.,
2012) or regard substance use or HIV-HCV co-infection as a challenge (Kamarulzaman and Altice, 2015 and Grebely and Tyndall, 2011); addiction treatment which limits access for people
with concurrent mental health and substance use disorders (el-Guebaly, 2004); exposure to correctional facilities which disrupt access to evidence-based care (Milloy et al., 2014); and
social and structural barriers such as stigma and discrimination, lack of housing, and fear of criminalization (Harris and Rhodes, 2013, Krusi et al., 2010, Neale et al., 2008, Treloar
et al., 2013 and Wolfe et al., 2010).”
SOURCE:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5086265/
Simply put: People who use substance experience a great deal of barriers and discrimination navigating healthcare systems simply because they use substance. In my role, I support individuals spanning from straight white men who find paperwork overwhelming, all the way to 2SLGBTQIA+ BIPOC with severe mental illness, physical illness and substance use. What all the people on my caseload find common ground on is that they all experience low income & poverty, and a great deal of suffering at the hands of corrupt systems.
At some point very soon, we need to come to terms with the idea that band-aid services are not the solution… but, as the Panther’s had it in the 60’s-80’s, they are simply survival programs
pending the revolution of new and just services for all people.


